Author: Lochon Maxime Alexandre Antoine
In 2020, at the height of the Covid-19 pandemic, some countries decided to lock down their populations. During this period, the living environment of millions, or even billions of people was constrained to indoor spaces. The SARS-CoV-2 virus, which is responsible for the Covid-19 disease, is part of the family of airborne viruses, and as such it is easier for this type of virus to spread and infect healthy people in closed spaces. Thus, limiting the spread in such spaces is a major challenge.
Each building has its own parameters that influence indoor air quality. Occupancy, ventilation, humidity, temperature, and physical activity are factors to consider in limiting the spread of airborne viruses.
This article will describe the links between the spread of Covid-19 and indoor air quality and will propose preventive measures to prevent its transmission.
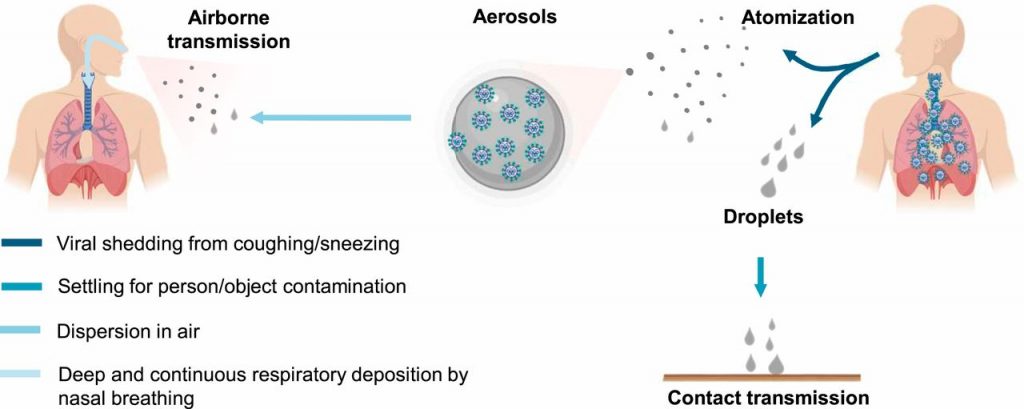
Transmission routes of SARS-CoV-2
Covid-19 disease is transmitted in the form of droplets (particles around 5 μm). These droplets are ejected from the respiratory tracts and spread through the air during a conversation, or following a cough or a sneeze. Then these droplets settle on surfaces and objects that will be handled by a healthy person or directly inhaled during breathing. It is at this moment that individuals are infected. [1]
Research has shown that the lifespan of SARS-CoV-2 is not the same depending on indoor climate conditions. Low humidity combined to low temperature can increase the vitality of SARS-CoV-2 in an aerosol. [2]
Also, depending on parameters like, air speed, temperature, and relative humidity (RH), the movement of the droplets is influenced. The droplets containing the virus can thus travel up to 10 m. These discoveries make indoor environments sensitive areas with increased risks of transmissions. [3]
Preventive measures to limit transmission in indoor environments
It is important to set up preventive measures in closed environments as they represent an increased risk of transmission of SARS-CoV-2.
To reduce the risk of contamination, key measures such as physical distancing and the use of properly worn masks are necessary. However, they may not be sufficient in overcrowded spaces where the exposure time is prolonged (>15 min) and with significant physical activity, for example: gyms or choirs. Indeed, physical activity can increase the expiration of infected respiratory fluids. For example, a normal breathing child aged from 7 to 9 years old generates around 14 liters of CO2 per hour, but a 15 years old teenager practicing a moderate physical activity can release up to 85 liters of CO2 per hour. Around 6 times more liters of CO2 are produced by the teenager. This shows that physical activity is an important parameter to consider. [4]
A possible solution can be provided by portable CO2 monitors (10cm x 10cm). They can assess the risk of contamination. We know that CO2 works as a proxy, and as such its concentration is correlated to the concentration of infected droplets in the air. A CO2 concentration threshold level of 700 ppm is proposed. Once this level has passed, ventilation of the space by opening windows and doors is necessary. [4]
In addition to this monitoring system, controlled mechanical ventilation devices (CMV) can be installed to guarantee correct and constant air exchange without the need to open doors and windows. When choosing centralized systems, it is important to take into account the problem of disinfection of the air ducts. To overcome this issue air purifiers which are capable of killing viruses can be installed. However, it must be verified that the air purifiers devices are using specific filters like high performance HEPA filters or ULPA filters DFS capable of nanometric disinfectant filtration (removal of nanoparticles). [4]
Another more economical solution would be to use a continuous air extractor which can allow a huge air exchange by extracting indoor air from enclosed spaces. [4]
These preventive measures will reduce the transmission of the virus, however many public buildings, even hospitals, have ventilation systems which have negative consequences on the spread of the virus. [4]
A focus on air recirculation issues
Many studies concerning the problem of the spread of airborne viruses in indoor environments with heating, ventilation, and air conditioning (HVAC) systems have been carried out. The results are clear: the HVAC airflow improves the diffusion of infected droplets in the indoor environment.
To support this result computational fluid dynamics (CFD) simulations were performed. The simulation studied the spread of the airborne virus in a hospital waiting room following a coughing event. Three scenarios have been tested:
- Scenario A : without HVAC system
- Scenario B : HVAC system with nominal air-flow of 2020 m3/h for each diffuser
- Scenario C : HVAC system with a doubled air-flow of 4040 m3/h
The following image shows the spread of infected droplets 30 seconds after sneezing.
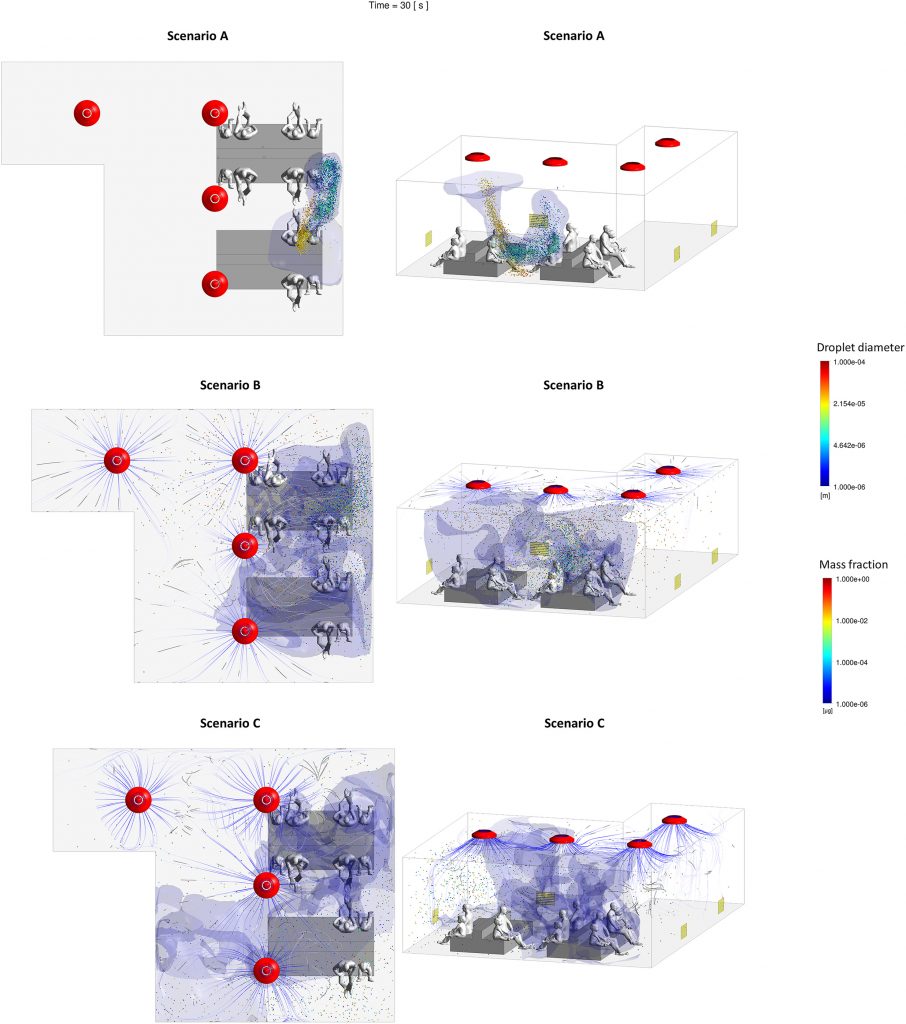
– Scenario A : Without HVAC system, Scenario B : HVAC system with nominal air-flow of 2020 m3/h for each diffuser, Scenario C : HVAC system with a doubled air-flow of 4040 m3/h [5]
It was deduced from the simulation that the spread of the virus increases with the air exchange rate.
Thus, the preventive measures seen previously are effective in preventing this problem. To improve indoor air quality, it is necessary either to use complex decontamination technologies or to avoid air recirculation by extracting indoor air. [5]
For hospitals, local exhaust ventilation (LEV) systems can also be used. The system consists of a tube with an air treatment unit with numerous filters placed above the patient bed. Such a system is quite appropriate inside patient rooms. The same study also looked at this equipment. To prove the effectiveness of the system, 2 scenarios were tested:
• Scenario A: basic situation, without LEV, the droplets spread thanks to the HVAC system.
• Scenario B: same situation but LEV system was placed above the spreader’s face.
The following image shows the effectiveness of the device. [5]
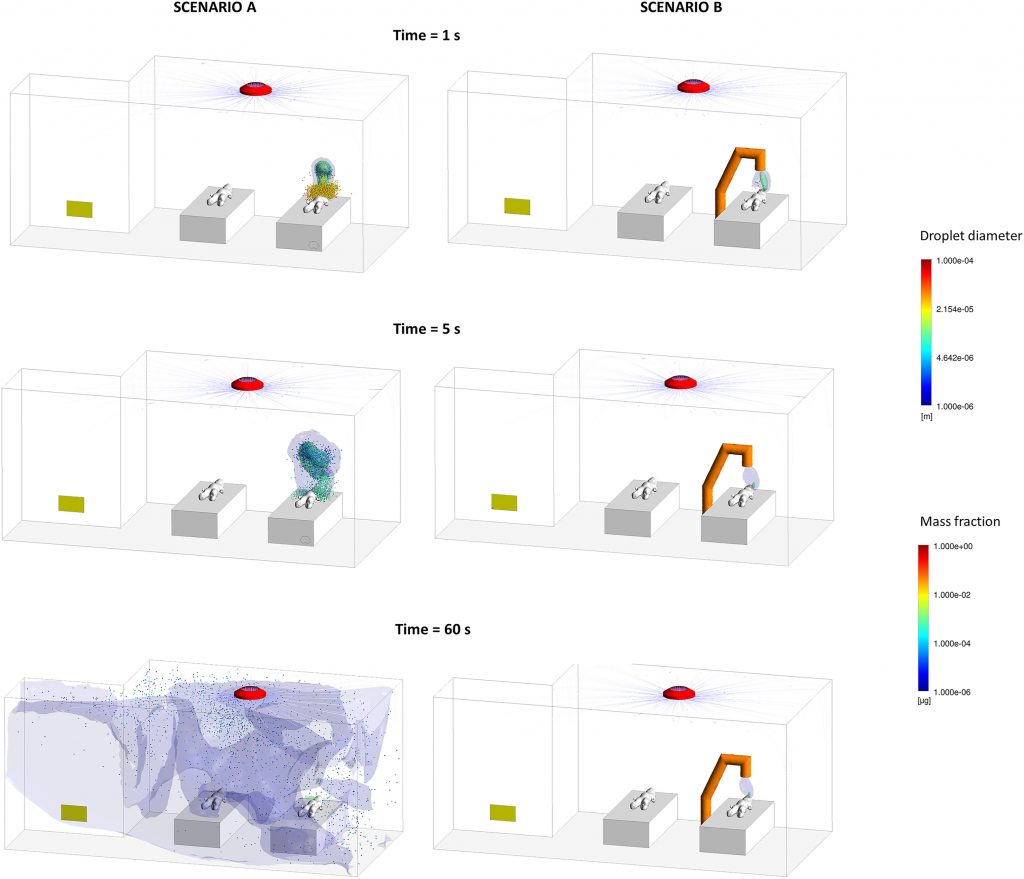
– Scenario A : without LEV system, Scenario B : with LEV system [5]
Conclusion
Since the arrival of Covid-19, the search for solutions of limiting the transmission of airborne viruses has been very active. Solutions have been found and must be set up if we want to avoid another pandemic of this magnitude. The Covid-19 disease had a huge impact on many aspects of our lives. The lessons of this pandemic must be learned to prevent us from reliving such a tragedy.
References
- [1] Zhang et al., “Identifying airborne transmission as the dominant route for the spread of COVID-19.”, 30.06.2020, Available at : https://pubmed.ncbi.nlm.nih.gov/32527856/ (Accessed : 01.05.2023)
- [2] Mecenas et al., “Effects of temperature and humidity on the spread of COVID-19: a systematic review”, 18.09.2020, Available at : https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0238339 (Accessed : 01.05.2023)
- [3] Maleki et al.,”An updated systematic review on the association between atmospheric particulate matter pollution and prevalence of SARS-CoV-2″, 04.2021, Available at : https://www.sciencedirect.com/science/article/pii/S0013935121001924 (Accessed : 01.05.2023)
- [4] P. Piscitelli et al., “The role of outdoor and indoor air quality in the spread of SARS-CoV-2: Overview and recommendations by the research group on COVID-19 and particulate matter (RESCOP commission)”, 08.2022, Available at : https://www.sciencedirect.com/science/article/pii/S0013935122003656#bib23 (Accessed : 01.05.2023)
- [5] Borro et al., “The role of air conditioning in the diffusion of Sars-CoV-2 in indoor environments: A first computational fluid dynamic model, based on investigations performed at the Vatican State Children’s hospital”, 02.2021, Available at : https://www.sciencedirect.com/science/article/pii/S0013935120312408 (Accessed : 01.05.2023)
- [6] “Role of Indoor Climate in Virus Transmission Mitigation”, 24.11.2020, Available at : https://www.epfl.ch/labs/hobel/role-of-indoor-climate-in-virus-transmission-mitigation/ (Accessed : 01.05.2023)
Feautured Image reference
image taken from the website : https://www.campusagri.fr/port-du-masque-obligatoire-a-linterieur-des-batiments/