Indoor environment has become the predominant habitat for urban individuals. Indoor air quality is therefore crucial for public health. Indeed, this confined air can expose us to chemical agents, pollutants and infectious agents.
The properties of each building such as location, occupancy or ventilation and indoor environmental factors including temperature, humidity, and airflow rates shape distinct microbiomes, in which airborne viruses pose a risk of contamination of the inhabitants. [2]
The problem of pathogens in the air in buildings has become particularly worrying with the emergence of the COVID-19 pandemic. In addition to the need to contain the coronavirus, social distancing measures and quarantines further increase the time ratio spent indoors from the usual 93% to 100% of the time for some, increasing the already prevalent importance of indoor air quality. [5]
This article will focus on engineering controls as measures to prevent the release of contaminants into the building. Engineering controls can be described as “a physical modification to a process, or process equipment, or the installation of further equipment”. [10]
Airborne spread of pathogens
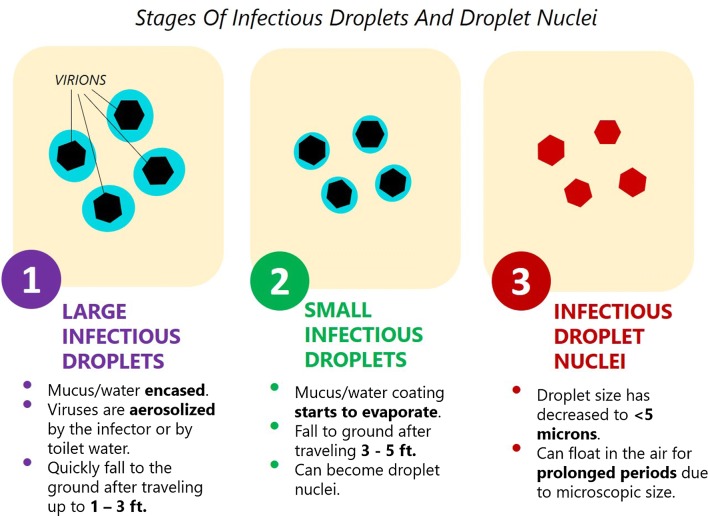
The passage of air from the lungs during coughing, sneezing or talking produces respiratory droplets of water ranging from 0.3 to 1000 microns that can contain viruses if the person is infected. [4] Airborne spread of pathogens consists of a process of atomization and then inhalation of droplet nuclei, formed by the dried respiratory droplets. [1] The virus-bearing aerosols become more dangerous when their size decreases, as the virus is less diluted in water and more active. They are more likely to enter the lungs and contaminate a person if they are smaller. [4]
Virus transmission occurs in two ways: through direct contact and airborne droplet transmission. [4] The respiratory droplets can stay in suspension in the air and be inhaled or settle on surfaces and contaminate individuals by contact transmission, e.g. an individual touching an object and then touching their face.

Aerosols containing infectious agents can be emitted from different sources, such as infected individuals or pets, as well as flushing toilets. Modelling work has revealed that large droplets could be expelled >6 m away by sneezing, >2 m by coughing and <1 m by normal breathing. The aerosols can be further propagated by indoor movements of air such as vacuuming or from a fan, also called air recirculation. [1]

With recirculation of the air, the airborne contaminants are transported from one space to another and infect new areas. Recent studies have established that COVID-19’s persistence in contact with a fluid or a surface can range from 3 hours (air) to 5 days (metal, teflon). [8]

Airborne microbial survival
A variety of indoor air parameters influence the survivability of airborne viruses. The most important of them are air temperature, relative humidity (RH), and turbulence. The effects vary according to the type of virus, but it can be noted that overall, an increase in temperature decreases the viability of viruses. The presence of certain gases such as ozone as well as UV light are harmful to viruses. Respiratory viruses survive best at lower RH (20%-30%) while rhinovirus viruses survive best at higher RH (70%-90%). [1]
Measures against airborne spread of viruses
Mitigating the drying of the droplets
An interesting approach in the regulation of the indoor climate to minimize the transmission of viruses is to avoid the drying of respiratory droplets into droplet nuclei by varying the parameters of the psychrometric chart. [4] This method has the advantage that it can be achieved using the conventional cooling and heating mechanism already present in many buildings.
By low temperature and low humidity, the respiratory droplets that are initially at human body temperature and high relative humidity undergo a size reduction due to heat and mass transfer potential, which increases the virus dangerousness as previously explained. The droplets become lighter and airborne, thus their floating time is significantly increased. [4]
It is therefore important to guarantee sufficient humidity and heat with the air regulation systems used in different climates. For example, in hot and dry climates, the drying potential for the droplet is high. If a cooling and dehumidification system is used in such a climate, the drying potential would be increased. A cooling with a humidification system like spray washer will improve the humidity level and will reduce the risk of viral contamination. [4]
Decontamination technologies
Various decontamination technologies are being developed, including UV irradiation or oxygen-based technologies such as ozone injection and plasma filtration. These technologies, although promising, are still not widespread. Their decontamination potential is often unfortunately not yet tested under scientifically valid conditions to be labelled by public health agencies. [1]
Controlling air recirculation
It has been demonstrated by experimental models that high air exchange rates facilitate dilution of the droplet nuclei that can contain viruses. [1] However, closed environments with poor air circulation favor concentrations of emitted aerosols, particularly in rooms dedicated to physical activity or social gathering. Bathrooms are also particularly at risk because flushing toilets can disseminate pathogens in the air. Proper ventilation of buildings is therefore crucial against the spread of airborne viruses. [4]
To fight the air recirculation problem, it is crucial to improve Indoor Air Quality (IAQ) by either avoiding air-recirculation through the opening of outdoor air dampers and closing the recirculation dampers, or dealing with it by using decontamination technologies such as particulate filters and regularly cleaning surfaces with disinfection equipment.

Nonetheless, in the interest of thermal comfort, opening outdoor air dampers in cold climates must be complemented by increasing the heating. [3] [5] The air-recirculation issue is more likely to happen in public buildings, where ventilation is not at the heart of financial investment, but can also occur in hospitals now, with the recent creation of very large emergency rooms where ventilation is not clearly established as sufficient for the situation.
Conclusion
There is an urgent need to develop indoor air control procedures to lower the risk of exposure and contamination. The COVID-19 pandemic and our lack of preparedness against viruses further underscores the magnitude of this threat.[1] Since airborne transmission is the most likely mechanism of infection, indoor air is a very important vector for the spread of airborne viruses. The understanding of the transmission processes and the development of control measures and infection prevention is more important than ever to contain the coronavirus pandemic. [1]
References
[1] Ijaz, K., Zargar, B., Wright, K., Rubino, J., Sattar, S., & Bact, D. (2016). Generic aspects of the airborne spread of human pathogens indoors and emerging air decontamination technologies. In American Journal of Infection Control, Volume 44, Issue 9, Supplement, 2 September 2016, (pp. S109-S120).
[2] Leung, M., Tong, X., & Lee, P. (2019). Indoor Microbiome and Airborne Pathogens. In Comprehensive Biotechnology, 3rd edition, Volume 6, (pp. 96-106).
[3] Morawaska, L., Tang, J., Bahnfleth, W., Bluyssen, P., Boerstra, A., Buonanno, G., Cao, J., Dancer, S., Floto, A., Franchimon, F., Haworth, C., Hogeling, J., Isaxon, C., Jimenez, J., Kurnitski, J., Li, Y., Loomans, M.G.L.C., Marks, G., Marr, L. & Yao, M. (2020). How can airborne transmission of COVID-19 indoors be minimised? In Environment International 142, 105832.
[4] Antony Aroul Raj Va, Velraj Rb, & Fariborz Haghighat (2020). The contribution of dry indoor built environment on the spread of Coronavirus: Data from various Indian states. In Sustainable Cities and Society, Volume 62, 102371.
[5] Abouleish, Mohamed (2020). Indoor Air Quality and Coronavirus Disease (COVID-19). In Public Health.
[6] “Severe acute respiratory syndrome coronavirus”, 2019 (Last modification: 5 October 2020), Wikipedia, Available at: https://en.wikipedia.org/wiki/Severe_acute_respiratory_syndrome_coronavirus (Accessed: 18 October 2020).
[7] Zhang, R., Li, Y., Zhang, A., Wang, Y., & Molina, M. (2020). Identifying airborne transmission as the dominant route for the spread of COVID-19. In Proceedings of the National Academy of Sciences of the United States of America (PNAS).
[8] Carraturo, F., Morelli, M., Cerullo, V., Libralato, G., Galdiero, E. & Guida, M. (2020). Persistence of SARS-CoV-2 in the environment and COVID-19 transmission risk from environmental matrices and surfaces. In Environmental Pollution 265, 115010.
[9] Lockhart, S., Duggan, L., Wax, R., Saad, S., Grocott, H. (2020). Personal protective equipment (PPE) for both anesthesiologists and other airway managers: principles and practice during the COVID-19 pandemic. In Nature Public Health Emergency Collection. Europe PMC.
[10] OSHWiki: Networking knowledge https://oshwiki.eu/wiki/Engineering_controls (Accessed: 18 October 2020).